Diagnosing - Complete blood count
A complete blood count is a basic blood test to determine the patient's health. It allows for the detection of infections, inflammations and shortages or excesses of particular types of blood cells, which may indicate a developing blood cancer.
Based on the blood count it is possible to detect not only different types of leukaemia, but also other hematopoietic diseases such as thrombocytopenia, polycythemia, some lymphomas and myelomas, or primary myelofibrosis.
Complete blood count is a basic test, which means that additional detailed examinations are necessary in order to make a precise diagnosis.
Bone marrow biopsy
A bone marrow biopsy is a basic examination that is performed in the process of diagnosing hematopoietic diseases. There are two types of bone marrow biopsies - fine needle aspiration biopsy and percutaneous trepanobiopsy.
Molecular and cytogenetic tests
Molecular tests
FISH (Fluorescence in situ hybridization) technique is used to determine the position of a specific gene on the chromosome. During cell divisions, it can be transferred incorrectly (e.g. translocation, inversion) or split into two pieces, which are then situated at opposite ends of different chromosomes. This marking technique relies on the fact that the DNA is complementary, i.e. the second strand is a mirror image of the first one and only for this reason can they bind together. When marking a gene, a complementary strand is created and then chemically combined with a fluorescent dye. A suspension of those markers is introduced into the tested cells. The complementary strands bind together and the excess markers are washed away. Then the cell is illuminated with laser light and the position of marked genes on the chromosome is observed under a microscope. By comparing it with the correct position, it is possible to see what mutation occurred in the gene.
The PCR technique allows infinite generation of a given DNA fragment. This allows doctors to not only determine whether a specific gene is present in the genome, but also to check whether a mutation has occurred in its internal structure. That method has significantly increased the knowledge of mechanisms leading to the development of leukaemia.
Cytogenetic testing
The method allows for a complete diagnosis of leukaemia, precisely identifying the lesions that cause a given type of disease. Through cytogenetic tests, chromosome aberrations (disorders) are determined, i.e. alterations that have occurred in the genome of leukemic cells. In addition, it is possible to determine the karyotype, i.e. full image and number of chromosomes in individual cells. It is the chromosomes that contain DNA genetic material, which acts as a carrier of the organism's genetic information and is identical in all cells, except for germ cells. In every mature cell that no longer undergoes division the DNA is found in its nucleus as loosely contained structures. When a cell is to divide, DNA condenses and forms 46 chromosomes, namely 23 pairs. There are two copies of genetic material, half from the mother and half from the father. The chromosomes seem to look the same and no differences can be seen when looking at them. However, chromosome pairs differ in size and degree of DNA condensation.
For tests, young cells that have the ability to divide are taken and, if leukemia is suspected, the bone marrow is taken. When cells start to multiply and chromosomes are already visible in their nuclei, the process is stopped using a special preparation. The nucleus of the cell breaks and the chromosomes, having more space, separate from each other. After adding a special staining preparation, characteristic striations are visible on the chromosomes, showing different degrees of DNA condensation.
Standard therapies - radiotherapy and chemotherapy
Chemotherapy
Chemotherapy is the most common method of treating cancers, including haematopoietic cancers. This type of treatment uses one or more cytostatic drugs that have a systemic effect, i.e. on the cells of the body, in particular on the cells that divide rapidly. Apart from cancer cells, during chemotherapy, other healthy cells that generally divide rapidly (bone marrow, skin cells, gastrointestinal mucosa) are also damaged. Chemotherapy is usually undertaking together with other treatments, including radiotherapy, hormone therapy, immunotherapy and surgical procedures.
Chemotherapy, depending on the type and severity of the disease, should assumecan:
- Completely cure the disease caused by neoplastic changes
- Stop the disease progressing
- Delay the progress of the disease
- Improve the patient's quality of life by alleviating some of the symptoms of the disease
The effectiveness of chemotherapy may vary.
A total response where all symptoms disappear (the patient feels and observes improvement and is confirmed by additional tests) is most desirable. The response to cytostatic treatment may also be incomplete when the treatment is working, but is only partially effective. Sometimes the body reacts to chemotherapy by stabilizing the disease, which does not progress but also does not regress. In some cases cancer progression is observed despite the cytostatic treatment applied.
Stem cell transplantation
Hematopoietic blood stem cell transplantation is carried out in the treatment of both cancer and non-cancer blood diseases. Hematopoietic stem cells are taken from related or unrelated donors and then given to the patient. This type of transplantation is known as allogeneic.
Auto blood stem cell transplantation, which is the administration of a patients' own cells, is also possible. Before the procedure, the patient receives intensive anticancer treatment. The patient's own hematopoietic cells can then enable the rebuilding of bone marrow and the proper blood composition to be restored.
Hematopoietic blood stem cell transplantation is a complex, multi-stage procedure. Patients stay in hospital for up to one month, followed by further treatment that take place at home and can last up to several months. If there are complications, all stages are longer.
Transplantation of bone marrow from a related or unrelated donor
The whole process starts with a pre-qualification stage carried out in the transplant center where the procedure is to be performed. The suitability of transplantation is assessed and the risks associated with it are determined.
The next stage consists of a thorough examination of the patient to assess organ capacity and exclude risk factors that could have a negative impact on the course of the transplantation itself, as well as the post-transplantation period. Upon successful completion of that stage, the search for a donor begins with the highest possible degree of HLA matching with the recipient. The patient's siblings are considered first, but only approximately 30% of patients, find a matching donor in their family. In addition, some family donors may be unable to donate for other reasons, such as medical reasons, making it even less likely to find a family donor. If patients are not able to find a donor within their family then the search continues for an unrelated donor on stem cell registries around the world.
Anyone between the ages of 18 and 55 and in general good health may be eligible to register with DKMS as a blood stem cell donor. Exclusions can be caused by certain chronic, genetic, autoimmune, infectious diseases. In Poland, up to 80% of patients find an unrelated donor.
In preparation for transplantation, patients must undergo a conditioning stage, which includes aggressive chemotherapy and if necessary, radiotherapy to destroy as many cancer cells as possible. Unfortunately, the patient's normal bone marrow is also destroyed. At this stage, it can only be rebuilt by a blood stem cell transplantation.
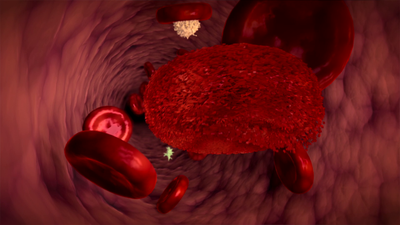
This stage sometimes leads to a dramatic, temporary decrease in blood morphology parameters. The number of white blood cells responsible for fighting infection is significantly reduced, the number of platelets ensuring proper clotting decreases, as well as the number of red blood cells that transport oxygen in the body. The patient usually needs to receive blood transfusions.
The next step is the transplantation itself, which involves transplanting the donor's hematopoietic blood stem cells to the patient. The procedure looks like a simple blood transfusion, lasting from several minutes to an hour. In 80% of cases the transplantation material (bone marrow hematopoietic stem cells) is collected from peripheral blood, in 20% from the pelvic bone.
After the procedure, the post-transplantation period begins, i.e. the time for engraftment. After 14-30 days if new white blood cells have appeared in the peripheral blood, then there is no need to continue with blood transfusions. It is also a sign that the transplant has started to work and the bone marrow is starting to function correctly.
During this particular waiting period, the patient's immune system is extremely weak and the risk of possible infections and infectious complications is very high. Patients must be kept in isolation and must carefully stick to stick regulations to protect them from the possible risk of infection. Even the smallest infection can be very dangerous and requires immediate attention.
While waiting for the engraftment patients may experience pain in the bones and joints caused by inflammation of the gastrointestinal mucosa. However, when new blood cells start to appear, the patient's condition improves dramatically. When a sufficient number of normal blood cells are present in the blood and the patient's condition is stable, the patient can be discharged from hospital, but must typically visit the transplant centre once a week for check-ups and possible transfusion of red blood cells or platelets. Those visits become increasingly less frequent three months after transplantation.
Autologous blood stem cell transplantation
In this case, the patient is both a recipient and a donor of blood stem cells. The patient's remission of the disease is induced and during that time hematopoietic blood stem cells are collected and frozen. After some time, conditioning, i.e. preparation of the patient with high-dose chemotherapy and/or whole-body radiation, is carried out. The next step is to transplant the patient with their own, frozen blood stem cells, which are used to regenerate blood.
Autologous transplantation has no anticancer effect, which results from activity of immune cells. It is also not associated with such high risk of complications, as in the case of transplantation from related or unrelated donors.
Hematopoietic blood stem cell transplantation is a method that gives the hope of a cure for many blood diseases. It improves the prognosis in certain types of leukaemia. It is a complicated process and burdensome for the patient's body, but this method also gives a chance to be cured of a serious disease.